In April 2022, mandatory calorie labelling in the out-of-home food sector (OHFS) was introduced in England as part of the UK Government’s strategy to combat obesity. The policy aims to provide the public with the information “they need to make healthier choices” and requires businesses with 250 or more employees selling food for immediate consumption to display the energy content of unpackaged food and non-alcoholic beverages in kilocalories (kcal), as well as contextual kcal reference information (1).
Previously mandatory calorie labeling on menus was introduced in parts of the United States, Canada, and Australia in the OHFS between 2018 and 2019. Calorie labeling is expected to have modest effects on consumer behavior in terms of kcal purchased (2). Calorie labeling may also encourage product reformulation. A meta-analysis found that calorie labeling in the OHFS was associated with a statistically significant reduction in kcal (-15 kcal) per dish (2).
A public survey conducted by the Office for Health Improvements and Disparities found that 79% of the UK population supported the display of calories on OHFS menus (3). However, calorie labelling has also been criticised since its introduction. For example, an analysis of Twitter reactions to the introduction of calorie labelling found that 71.4% of 276 respondents expressed negative attitudes towards this policy (4). This partly reflected public concern about the impact of this policy on people with eating disorders. Calorie labelling has been criticised by BEAT, the UK’s leading eating disorder charity. It has been suggested that this policy increases the vulnerability of those at risk of developing an eating disorder, worsens eating disorder symptoms in people already diagnosed and perpetuates stigma related to being overweight (5).
What does research say about the potential impact of calorie labeling on people with eating disorders? Until recently, there was no shortage of studies on this topic, but a small number of new studies have attempted to answer this question. Four studies used qualitative methods to explore the opinions and experiences of people with eating disorders (see Table 1). Recurring themes describe how calories on menus can lead to an over-obsession with calories, limit food freedom (meals are chosen based on their caloric value rather than what one actually wants or what corresponds to feelings of hunger), reduce opportunities to eat out, increase feelings of anxiety, guilt, and shame about food choices, and hinder recovery from eating disorders. Some participants in these studies expressed anger at the message from “trusted” health authorities to normalize calorie counting because calorie counting had played a crucial role in the development of their eating disorders (6, 7). Although these qualitative studies predominantly list negative effects on eating disorders, some positive aspects have also been identified: calorie reporting can increase feelings of security, control and responsibility for the food consumed (7, 8), and for some people, the information provided can help reduce overconsumption and the resulting feelings of guilt (9). Others, however, perceived this control element as negative, as it increased eating disorders (7).
In these recent studies, quantitative data suggest some support for the policy. In one study measuring support for the policy, 43% of participants diagnosed with eating disorders were found to agree with the implementation of the policy (Table 1). When asked specifically about ED symptomatology, 55% (of 583 participants with ED) reported that calorie labeling could worsen their ED symptoms (8), and 91% (of 399 participants) reported that they had problems due to calories on menus (7).
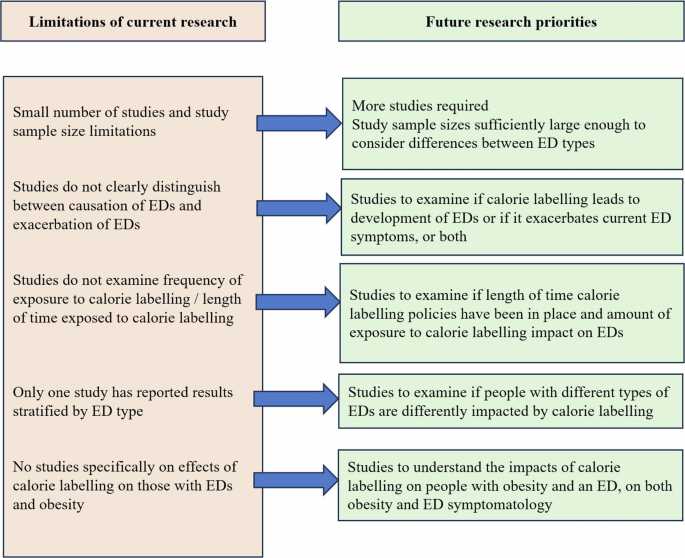
But what about measured objective changes in eating disorder symptoms as a result of calorie labeling? There is very little evidence to date, but a 2015 study attempted to examine the negative consequences of calorie labeling. Using a sample of 299 female college students considered at high risk for eating disorders, Lillico et al. (10) measured eating disorder scores, affective reactions (anxiety and body image satisfaction), unhealthy weight-related behaviors (binge eating, calorie restriction, excessive exercise), and calorie consumption before and after the introduction of calorie labeling in a university cafeteria. They found no significant differences in any of the measures whether calorie labeling was present or not, and concluded that calorie labeling had no negative effects on those at risk for eating disorders. However, it is important to note that although these participants are considered to be at high risk for eating disorders based on their age and gender, they were stratified by Eating Attitudes Test scores rather than a formal eating disorder diagnosis. Further research is therefore needed into the influence of calories on menus to see whether these findings are generalizable to people with diagnosed eating disorders. Similarly, further studies are now needed to develop the very minimal body of evidence outlined in Table 1, including further research into the effects on people with obesity and eating disorders, and to understand the effects on people with different eating disorder types (including binge eating, anorexia nervosa and bulimia nervosa) (see Figure 1).

Key research priorities regarding the impact of calorie labeling on eating disorders.
While the UK government’s guidelines on calorie labelling recognise that people with eating disorders may have difficulty seeing calorie information on menus and allow businesses to offer a zero-calorie menu upon request “at their discretion” (1), testimonials from people with eating disorders suggest that zero-calorie menus are not always available (11). For example, a recent observational study found that only 12% of 90 food and beverage establishments offered a zero-calorie menu upon request (12). In addition, the very act of requesting one can be distressing for people with eating disorders as it draws even more attention to their eating disorder (11). Perhaps the best solution would be for all establishments to make it mandatory to offer both calorie and zero-calorie menus, either online or via QR code (7), eliminating the need to publicly ask for a zero-calorie menu.
Eating disorders are complex mental illnesses. Many people with eating disorders also suffer from obesity, and obesity is also a risk factor for developing an eating disorder (5). Therefore, many people who are the ‘target’ of calorie labelling are at risk. Despite the perceived negative impact of calories on menus, many people with eating disorders understand the need to address obesity at a population level, and a significant proportion support calorie labelling. However, this should not come at the expense of their own health, nor should it reinforce overweight stigma or encourage restricted diets. As with any public health policy, we should first aim to ‘do no harm’. Based on studies conducted to date, we propose that businesses should be required to offer calorie-free menus alongside menus with calories.